At around the age of 40, Maja Olecka’s friend suddenly found she could no longer handle her drink. Quantities of alcohol that she would have shrugged off in the past now knocked her for six. Her hangovers got much worse.
Olecka’s friend certainly isn’t alone – when I was around that age, I heard similar stories from friends, many of whom quit drinking. But Olecka, a researcher at the Leibniz Institute on Aging – Fritz Lipmann Institute in Jena, Germany, thinks she knows why it happens.
At this age, she says, many people experience a rapid burst of ageing, altering their ability to metabolise alcohol. And that, unfortunately, isn’t all. This sudden ageing, reflected in dramatic molecular shifts, comes with an acceleration in muscle wastage and skin decline. Immune cells die off swiftly and there are substantial increases in the risk of cardiovascular disease and of dying. Research also suggests that this surge of ageing happens again, at around 60 and 80.
Ageing, it turns out, might not be the steady downhill slide from the uplands of youth to the perpetual après-ski in the sky we all thought. “Many contemporary definitions of ageing are describing it as a gradual, linear process,” says Olecka. “We have to abandon this assumption.”
Instead, it might be more like whitewater rafting: long stretches of calm punctuated by sudden periods of extreme turbulence, punching holes in your raft until you eventually sink. This surprising discovery is still at an early stage, but it could have profound implications – not just for our understanding of ageing, but also for our efforts to slow it down.
Ageing instalments
The first hints that ageing proceeds in instalments came from studying Smurfs – not the small, blue cartoon characters, but small, blue fruit flies.
In 2011, Michael Rera, then at the French National Institute of Health and Medical Research in Paris, discovered that flies from the species Drosophila melanogaster enter a distinct phase towards the end of their natural lives. Feeding the flies blue dye – initially as a way to measure their food intake – turned them blue, hence the name “Smurf”. But the flies only became blue after reaching a certain age: older fruit flies have leaky guts, so when they consume the dye, it seeps out into their body cavity, turning them blue.

Fruit flies age in two distinct phases
Aurore Colibert and Michael RERA
This blue state, and the intestinal permeability that causes it, is a reliable indicator that the fly is about to die – and soon. The flies enter Smurfdom very rapidly: one day they are fine, the next they are blue, and not long after, they are dead. The Smurf state is also characterised by some classic signs of decrepitude, including decreases in spontaneous motor activity (they move less) and energy stores. This led Rera – now at the Jacques Monod Institute in Paris – to propose that the Drosophila ageing process is biphasic, chugging along slowly for most of a fly’s adult life and then suddenly flipping into a profoundly more decrepit state. This may be because the flies can withstand the accumulation of molecular damage for a long time, but then hit a threshold that they can no longer bear.
Smurfdom has since been observed in other organisms, including nematode worms and zebrafish, hinting that the gut permeability it indicates is a common feature of ageing.
Humans, fortunately, don’t turn blue the closer we get to death. But over the past few years, evidence has accumulated that we, like fruit flies, experience similar rapid escalations in how we age, possibly for similar reasons.
In 2022, for example, a team at the Wellcome Sanger Institute in Hinxton, UK, discovered a major and rapid transition in the ability to make new blood cells around the age of 70. Up to that point, most people have a strong and stable population of 20,000 to 200,000 haematopoietic stem cells pumping out new red and white blood cells and platelets. But after 70, that drops precipitously, such that the majority of new blood cells are made by just hundreds or even tens of stem cells. This hugely raises the risk of anaemia and other conditions characterised by reduced blood cells, along with immune system dysfunction, poor tissue regeneration and blood cancer – all of which increase the risk of death and were already known to suddenly surge in the over-70s.
The cause of this abrupt collapse seems to be that most of these haematopoietic stem cells finally succumb to the molecular damage that has accumulated across their lifespan. According to Steve Hoffmann, Olecka’s colleague at the Leibniz Institute on Aging, this is a classic tipping point, when a system undergoes an abrupt shift from one equilibrium to another, often irreversibly, after a long, slow build-up of pressure.

The sudden burst of ageing at around 60 can come with increased risks of heart disease, Parkinson’s and Alzheimer’s
Martin Parr
The concept is familiar in physics, ecology and climate science, but Olecka and Hoffmann want to bring it into ageing research – carefully. “It’s a tricky term because there is no strict scientific definition of a tipping point and different fields use it in different ways,” says Olecka. “But I think it is a very good term to convey the general concept of abrupt change after crossing some threshold.”
Our ageing tipping points
Olecka and Hoffmann’s idea draws on mounting evidence that, in multiple areas and systems in the body, ageing processes are amplified after critical biological limits are breached. Researchers have uncovered other such tipping points, many of them at roughly the same age. In the late 2010s, for instance, a team led by Tony Wyss-Coray at Stanford University in California became interested in heterochronic parabiosis, a gruesome procedure whereby the circulatory systems of two animals are surgically connected. In a 2011 study, Wyss-Coray and his colleagues connected the circulatory systems of an ageing mouse and a young mouse, discovering that the procedure rejuvenated the old mouse and aged the young one. Their findings suggested that blood – or, more specifically its fluid portion, plasma – contains key regulators of ageing.
To see what those might be, he and his colleagues tracked how proteins in plasma change over the course of human ageing. In a study published in 2019, they took blood from 4263 people aged from 18 to 95 and measured the levels of 2925 proteins in the plasma. They expected to see gradual, linear changes with increased age, but they didn’t.
To their surprise, they found that the participants clustered into four groups: the under-34s, those aged 34 to 60, people aged 61 to 78 and the over-78s. Within each group, the protein profiles were very similar, but at the ages of 34, 60 and 78, they suddenly changed, with levels of some proteins rising dramatically while others plummeted. What’s more, some of the proteins that became enriched in the older age groups were already known to be associated with cardiovascular disease and Alzheimer’s. The researchers also found enrichment of a protein associated with Down’s syndrome. None of the participants had Down’s, but one consequence of the syndrome is accelerated ageing. Their conclusion was that humans appear to undergo three rapid pulses of ageing around the ages of 34, 60 and 78.

A rapid burst of ageing happens at around 80, with upticks in heart disease risk and markers of brain ageing
Martin Parr/Magnum Photos
In an even deeper dive, a team led by Michael Snyder at Stanford University looked at RNA, metabolites, lipids and inflammatory molecules as well as plasma proteins in 108 people aged between 25 and 75. The researchers found that molecules that were already known to be markers of ageing spiked dramatically during two brief windows, first in the early to mid-40s and then at around 60. Both spikes included molecules associated with an increased risk of cardiovascular disease, dysfunctional lipid metabolism (which can cause the harmful build-up of fats or fat-like substances in cells and tissue), decreased muscle stability and diminished skin integrity, rendering it more vulnerable to damage and infection. But both had unique features too. The first spike came with declines in the ability to metabolise caffeine and alcohol efficiently, explaining the middle-aged hangover problem. The second spike hinted at precipitous declines in kidney function and the immune system.
“What we discovered is that most things aren’t changing linearly,” says Snyder. Only 6.6 per cent of the thousands of molecules tracked with age; 81 per cent changed non-linearly. The fact that the timing of the spikes roughly corresponds to the first two seen by Wyss-Coray’s team at 34 and 60 suggests that they are picking up the same signals, he says. His team was unable to see if there was a spike at 78 because their oldest subjects were only 75.
Classic tipping points occur when a system undergoes an abrupt shift from one equilibrium to another
There are signs that individual organs and systems also age in stages. In 2020, for example, researchers in Germany made molecular profiles of skin samples taken from women aged 21 to 76. They found, unsurprisingly, that skin from older women had more molecular markers of ageing. But the journey from young to old skin is wrinkly, with tipping points at around 30, 50 and 65, segmenting skin ageing into four distinct phases. Tipping points have been discovered in the brain’s plasma proteome, the collection of proteins found in blood plasma, at 57, 70 and 78, coinciding with an increase in biomarkers of ageing. And some key immune system cells, including B-cells, T-cells and natural killer cells, experience two bursts of decline and ageing around the ages of 40 and 65, probably contributing to the weakening immune function that is a hallmark of ageing.
The tipping points may also underlie some hitherto puzzling patterns in the occurrence of age-related diseases and death. According to Snyder, we already know that the incidence of certain age-related diseases exhibits step changes. The risk of developing cardiovascular disease, for instance, increases from 16 per cent to 40 per cent at age 40, then stays roughly flat until age 59. The risk then jumps to about 75 per cent at 60, and again to about 85 per cent after 80. Similarly, the incidence of the neurodegenerative conditions Parkinson’s and Alzheimer’s accelerates first more gently at around 40 and then again more aggressively at roughly 65.
Mortality data also shows subtle non-linearities. The long-standing assumption is that mortality rates rise smoothly and exponentially throughout adulthood, such that the risk of dying from any cause doubles roughly every eight years. But when Aleksei Golubev at the N. N. Petrov National Medical Research Center of Oncology in Saint Petersburg, Russia, took a close look at data from France, Sweden and Japan, he unexpectedly found three periods where the mortality rate slightly but discernibly accelerates – around the ages of 17, 38 and 60. The first of these is probably down to extrinsic factors such as accidents, according to Hoffmann, but it is intriguing that the other two coincide with molecular tipping points. They may, therefore, be partly due to accelerated ageing at those times.
What causes a tipping point?
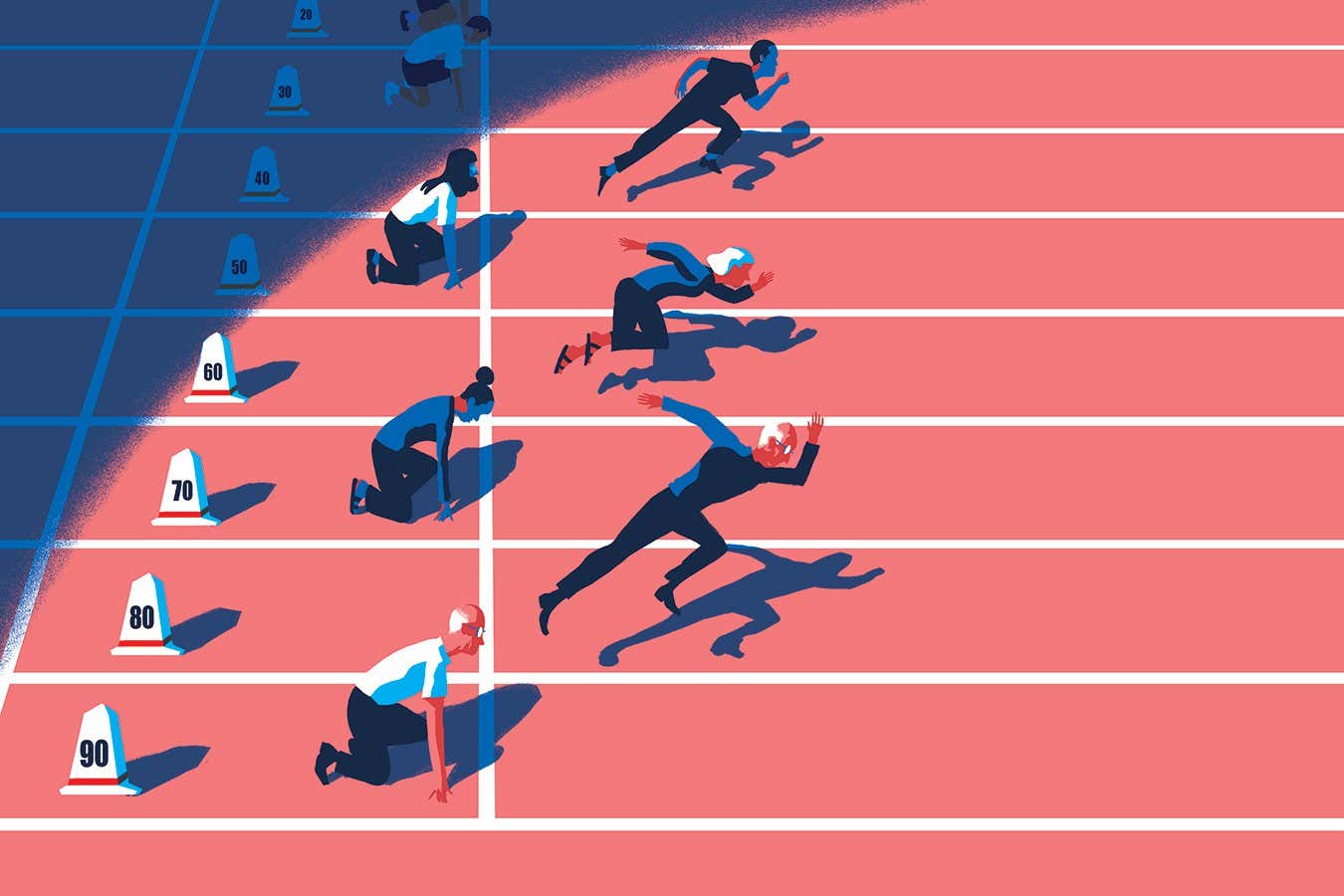
If you amalgamate all the ageing tipping points – making allowances for some outliers, such as skin ageing – it appears that once we reach maturity, our lives are roughly divided into phases lasting about 20 years. “I think we need more data, but from what I see, the most important transitions in humans are around 40, around 60 and then around 80,” says Olecka.
You might say we know that intuitively – we generally refer to these phases as young adulthood, early middle age, late middle age and old age (see “The ageing tipping points”, below). But research tells us that these informal labels are genuine life stages with distinct biological characteristics.

So, what precipitates these sudden shifts? According to Olecka and Hoffmann, it is probably accumulated molecular damage that eventually overwhelms the body’s ability to deal with it, not unlike what happens to the fruit flies. Our natural repair systems can buffer these molecular changes up to a point, but then become swamped or exhausted, causing the system to slump into a new state. This is hypothetical for now, but some possible buffers are DNA repair (the cellular processes that identify damage to DNA molecules and correct them), antioxidants and the molecular “chaperones” that ensure the correct folding of proteins. There could also be domino effects, where crossing one tipping point pushes another over the threshold, they say.
Snyder suspects that the transition around 40 is partly down to lifestyle changes. “My guess is that people are not exercising as much, they become more sedentary and they’re probably not eating as well,” he says, “and it catches up with them when they hit their early 40s.”
That holds out the prospect of delaying the arrival of tipping points with diet, exercise and, maybe one day, a new class of pharmaceuticals tentatively called “anti-transition agents”. Though not all ageing processes follow non-linear dynamics – mutation accumulation, for example, is linear – Hoffmann notes that “these non-linear transitions are exceptionally interesting”. Exploring them could open new targets for anti-ageing therapeutics.
“For now, people are looking for anti-ageing medication that would work for everyone, but maybe we should look for strategies to stop or delay the transitions,” says Olecka. “This may be a more successful and more targeted approach.” Such drugs are a long way off, but steps have already been taken in the form of genetic interventions that Rera’s team has designed to postpone fruit flies’ entry into the Smurf state.

Diet and exercise might be key factors in delaying our ageing transitions
Paul Glendell/Alamy
In the meantime, Olecka and Hoffmann envisage translating the basic research into a stratification system for ageing, whereby people are assigned to one of the four, or maybe even five or six, stages and treated accordingly. “We think that the transitions may mark natural boundaries between stages of ageing and be useful for prevention,” says Olecka. “Some interventions may be beneficial in a younger stage, but be detrimental in the older stage of age.” Again, though, the specifics await discovery.
So once the Rubicon has been crossed – after an age stage has been reached – is there any going back? “This is a very, very important question to answer,” says Olecka. “We don’t know yet.”
But we could know soon. Snyder, for one, is crunching data from a bigger group of people he followed for 12 years. One of his aims is to find out which interventions might delay the tipping points. “By tracking people’s lifestyles, we’ll get a better feel for if some people are able to push these changes into their 50s or later,” he says. “And if so, what were they doing to make that happen?”
With the accumulation of such compelling evidence and new research under way, as Hoffmann says, the field of ageing research may itself be approaching a tipping point.
Topics: